Amniotic Membrane How-To: Techniques for In-Office and Surgical Use
From severe dry eye disease to delayed healing, here’s how this procedure benefits patients
Karl G Stonecipher | | 6 min read | Practical
For challenging cases with corneal surface damage, we have traditionally performed punctal occlusion, patched the eye, and then ordered some antibiotics. Now, we can add amniotic membranes into our armamentarium as a therapeutic intervention to help the eye heal faster.
Amniotic membranes control inflammation, promote healing, reduce scarring, and can improve visual acuity as the corneal surface heals (1,2,3,4). And they are not just for anterior segment surgeons – far from it; they can be used by both ophthalmologists and optometrists for defects (various corneal ulcers and severe dry eye disease), delayed healing (keratoconjunctivitis or keratitis), dystrophy (epithelial or recurrent corneal erosion), degeneration (band keratopathy, nodular corneal degeneration), and damage (chemical, thermal, and acid burns, Stevens-Johnson syndrome).
We can insert an amniotic membrane in a simple in-office procedure or apply it in the surgical suite to promote postoperative healing. Either way, the procedure is reimbursable for multiple diagnostic codes with a documented ocular surface defect (CPT code 65778, average Medicare $1,400, private insurance $900-$1,300) and so it is a welcome addition to any practice.
Back to basics: What is an amniotic membrane?
The amniotic membrane is a layer of tissue derived from placentas donated by mothers undergoing planned C-section deliveries. The placenta’s amniotic membrane layer is selected for use in the eye because it is acellular and immune privileged, avoiding an immune response that can hinder healing (5). The amniotic membrane is made up of extracellular substrates, including collagen, elastin, glycosaminoglycans, and fibronectin. This reservoir of bioactive components encourages healing and epithelial cell migration while inhibiting scarring, angiogenesis, inflammation, and microbial growth (1, 2, 3, 4).
When the amniotic membrane is prepared for clinical use, it can be processed naturally, without any harsh chemicals. One option, AcellFX, is air dried and ready to use right out of the package – either alone or under a contact lens. Another amniotic product in the market is Prokera (BioTissue), which is maintained in moisture and stretched across a malleable ring.
How to implant amniotic membrane
Among the categories of pathology that we treat with amniotic membranes, defects and delayed healing are most commonly treated in-office, while we often also treat postoperatively for dystrophy, degeneration, and damage. In my experience, the membrane lasts 3-5 days on the eye in most cases and works over 6-10 days.
We follow two basic techniques: place or place then cover. The first simply entails placing the membrane in the fornices, where it adheres and goes to work. It’s an appropriate technique in many cases, including cases involving an active infection. In place and cover, we cover the membrane with a bandage contact lens, which allows longer healing time and makes it more comfortable to apply topical medication. Cases of active infection usually rule out a bandage contact lens. I can use AcellFX with both techniques, whereas Prokera has an integrated ring that helps keep the membrane in place for a place-and-cover effect.
To apply the amniotic membrane, first I place an anesthetic drop in both eyes and clean the eyelid with lid scrub solution. With the eye held open by an assistant or a speculum, I dry the cornea with a sterile spear sponge and debride if needed. For a place technique, I grasp the membrane with sterile forceps and place it deep in the lower fornix, smoothing with a dry surgical spear to establish contact. Using the place and cover technique, once the eye is prepared, I remove excess water from a bandage contact lens, place the membrane on the lens, and place the lens on the eye, pressing it gently in contact. I patch the eye and see the patient back the next day. An amniotic membrane is applied the same way in the surgical suite – and postoperative care and follow-up follow the normal routine, along with the following home care instructions that I give to all amniotic membrane patients:
- Patients use an artificial tear with hyaluronan every two hours while awake for two days, followed by every four hours on days 3–6.
- Patients apply moist heat therapy at least 2–3 times a week starting at week four, and then drop to once per week after two months.
- Patients use a mild facial cleanser or eyelid hygiene solution daily for ongoing maintenance.

Credit: Collage images sourced from Unsplash.com
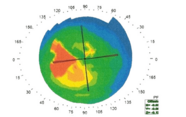
Three cases
Severe dry eye disease: A 65-year-old woman was unresponsive to standard therapy for dry eye disease, including cyclosporine and thermal pulsation. She presented with an OSDI score of 63 and lissamine green staining across the board (4-4-4). I inserted AcellFX at the slit lamp, placed in the lower fornices with no contact lens cover. She followed my home care instructions (above) and returned at one week showing improved appearance and quieting of inflammation. At one month, her OSDI score was 23 and her staining was clear.
Poor corneal healing after cataract surgery: A 75-year-old woman experienced poor healing in the left eye after cataract surgery, followed by corneal failure after cataract surgery in her right eye. Immediately after the second surgery, I placed one AcellFX membrane in the right eye with a bandage contact lens and another in the inferior fornix of her left eye. Where it took several weeks to attain her final vision in the left eye, the prophylactic approach for the right eye reduced her rehabilitation time to just two days beyond normal healing.
Acute intervention after trauma: A 23-year-old male working for a cleaning service suffered severe exposure to an ammonia cleaning agent. In the emergency room, he had corneal irrigation with a Morgan lens using a 0.9% sodium chloride injection USP until the pH was neutral. He was referred to my office and taken immediately to our minor operation suite. I inserted a Prokera ring 6.0 mm, placing gatifloxacin 0.5% before and after insertion. I prefer the Prokera ring in such cases because it maintains the fornices in an anatomical position that is best for accelerated healing. Without the ring in this type of case, I’ve found that patients can have excess scarring of the fornices. The patient healed completely and was able to quickly return to work.
A breadth of benefits
Given the breadth of clinical applications for amniotic membranes, this is just a glimpse of the patients who can benefit. If you want to start using them in your office or surgical suite, the learning curve is short and the manufacturers offer quality resources and support.
- D. Meller et al., “Amniotic membrane transplantation in the human eye,” Dtsch Arztebl Int. 108, 243, (2011) PMID: 21547164.
- A. Walkden, “Amniotic membrane transplantation in ophthalmology: an updated perspective,” Clin Ophthalmol, 14, 2057, (2020) PMID: 32801614.
- JP. Craig et al., “TFOS DEWS II definition and classification report,” Ocul Surf, 15, 276 (2017) PMID: 28736335.
- L. Jones et al., “TFOS DEWS II management and therapy report,” Ocul Surf., 15, 575 (2017) PMID: 28736343.
- DE. Fetterolf, RJ Snyder, “Scientific and clinical support for the use of dehydrated amniotic membrane in wound management” Wounds, 24, 299, (2012) PMID: 25876055.
Karl G. Stonecipher, MD, is a Clinical Professor of Ophthalmology at the University of North Carolina, a Clinical Adjunct Professor of Ophthalmology at Tulane University, and Medical Director for Laser Defined Vision in Greensboro, North Carolina.
Disclosures: Dr. Stonecipher is a consultant for BioTissue, Thea, and Verséa Biologics.