Glaucoma Under Pressure
Serial entrepreneur Barbara Wirostko, M.D. FARVO, walks us through a novel therapeutic approach that tackles EVP
Jon Greenaway | | 5 min read | Interview
The last two decades have seen an explosion in treatment options for glaucoma – from new pharmacotherapies to the increasingly popular (minimally invasive) surgical intervention. But despite all the exciting developments, there is still more to do, attracting the attention of savvy clinician-researchers and business innovators who know the need and potential market. Here, ophthalmologist and entrepreneur Barbara Wirostko, M.D., explains how episcleral venous pressure (EVP) could expand the glaucoma armamentarium.

Meet Barbara Wirostko
I’m Barbara Wirostko – a fellowship trained glaucoma specialist, board-certified by the American Academy of Ophthalmology (AAO). I’m also a Gold Fellow with the Association for Research in Vision and Ophthalmology (ARVO), and I serve as an adjunct professor of ophthalmology and biomedical engineering at the John A. Moran Eye Center at the University of Utah.
I describe myself as a clinician-researcher as well as a serial entrepreneur, and I am currently the co-founder and chief medical officer (CMO) of Qlaris Bio – a biotechnology company that targets high unmet needs in debilitating ophthalmic diseases. I’m also the co-founder and CMO of a start-up called MyEyes, which aims to help patients get access to an at-home tonometer.
I see patients at my clinical practice in Park City, Utah, and work at the Salt Lake City Veterans Administration Hospital as an attending physician at the glaucoma clinic, where I teach fellows, residents, and medical students.
When it comes to my business activities, what unites all my projects is a love for being creative, innovative, and building teams that have the freedom to tackle big problems. If you build a team with that aim, you get to see people develop – and watch them conceive exciting ideas.
What are your company's aims?
When I co-founded Qlaris Bio in August 2019 with Thurein Htoo, MS, MBA, – a former colleague from Pfizer, we had a singular premise in mind: To develop better solutions for patients suffering from debilitating ophthalmic diseases.
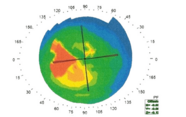
We started the company based on the innovative research of Professor Michael Fautsch, Ph.D., of Mayo Clinic, who had been working on ATP-sensitive potassium channel openers as vasodilatory agents for lowering intraocular pressure (IOP). He discovered that these agents worked on a very unique portion of the Goldmann equation – episcleral venous pressure (EVP). Since the introduction of MIGS, the field has been running into a problem; we can lower IOP, but it seems like we can only lower it so much. This pressure floor is likely due to EVP’s impact on the outflow system, which is exactly what the potassium channel openers target. Our developmental compound QLS-111 specifically targets EVP to treat various forms of glaucoma.
Could you share a few more details about your novel compound?
What is unique about this compound is that it works with physiology and doesn’t disrupt the normal tight junctions of the vasculature. As a result, we have a great safety profile – we don’t see any clinically relevant hyperemia – and the results on efficacy are extremely promising. We are currently entering Phase II trials for normal-tension glaucoma (NTG) and primary open-angle glaucoma (POAG).
Beyond QLS-111, what other avenues are you exploring with Qlaris Bio?
We have known that EVP played a role in the progression of diseases like Sturge-Weber syndrome, but we didn’t appreciate to what extent EVP also plays a role in the progression experienced by POAG and NTG patients. It wasn’t until we had the breakthrough of MIGS – when we really did expect the pressure to be lower than what was achieved – that the picture became clearer that the limiting factor was EVP. And that’s a good lesson; every time we take a step forward in treatment options, we have to confront the fact that new problems and learnings may be encountered.
What does the future of glaucoma treatment hold?
I would love to be able to offer patients continual IOP-lowering therapeutics – whether that's laser, surgery, or medication. I think it all has a place.
When it comes to medication, tolerability and compliance are problems for multiple reasons. Patients can and do really struggle with a multi-drop regimen and often end up with ocular surface irritation and hyperemia, leading to non-adherence.
In the next 5–10 years, I believe we will be moving toward continuous IOP control. Whether that be longitudinal across months/years or simply better 24-hour IOP lowering therapeutics, we need less fluctuation and far better control. The other important area will be understanding not only the unmet needs associated with EVP, but also the genetics, so we can treat or even cure glaucoma. Of course, these efforts will develop alongside other areas, such as neuroprotection or neuro-regeneration.
I think those three: continuous and sustained IOP control, genetic identification and approach, and neuro regeneration/protection are the three holy grails of glaucoma in the coming decade, and I can’t wait to see what we come up with next!
Ophthalmology has several good examples of high-profile start-ups shaking up the field. What makes the field so dynamic?
In ophthalmology, we get to draw from every therapeutic area. With antibiotics and anti-infective agents, we draw from the infectious disease space. Timolol, a beta blocker, we drew from cardiology. And for devices, we work with engineering. Just think about anti-VEGF drugs, which have revolutionized how we treat wet AMD – that’s ophthalmology borrowing from oncology. It’s a unique field that combines surgery and medicine, and given the nature of ocular diseases, we need innovative devices, drugs, and procedures to treat people. I think this inspires people to get creative!
When did you decide that ophthalmology was for you?
I remember the exact moment. My father, Emil Wirostko, M.D., a uveitis specialist at Columbia Presbyterian Medical Center, was my biggest role model. I started doing research with him back when I was in high school, so I knew from a young age that I wanted to be a physician. I would later do my training at Columbia, and, during my third year there, I was doing my ophthalmology rotation and we learned how to use an ophthalmoscope. I vividly remember that moment of looking into one of my colleague’s eyes and visualizing the retinal blood vessels and the optic nerve in such detail. From that moment on, I fell in love with ophthalmology.
After almost a decade working in academic writing, I wanted to find a new challenge that would let me keep telling stories, learning new things and experiencing the excitement of scientific innovation. That’s what makes The Ophthalmologist a perfect fit for me.