One Size Does Not Fit All
Important factors to consider when selecting premium IOL technologies for patients with glaucoma

Credit: Image sourced from Pexels.com
The micro-invasive glaucoma surgery (MIGS) revolution has ushered in completely new thought processes about glaucoma management. Many of the new MIGS options are performed at the time of cataract surgery. Given that they can be performed ab-interno through the same temporal clear corneal incision as the phacoemulsification, there is little change in surgically induced astigmatism, resulting in predictable and consistent refractive outcomes in most cases.
Although newer, advanced intraocular lens (IOL) technologies can come with known risks including glare, haloes, or loss of contrast sensitivity, mild to moderate glaucoma patients with the well-controlled disease need not automatically be dismissed when it comes to so-called premium IOLs.
What are the main IOLs?
Toric IOLs can be considered in patients with reasonable visual potential regardless of severity or type of underlying eye pathology. Toric IOLs help maximize visual acuity and avoid distortions or asthenopia common with spectacle-based astigmatism correction, without the additional risk of glare, halo, or reduced contrast sensitivity. On the other hand, the multifocal IOLs today use diffractive optics to create multiple focal points on the retina, meaning that less total light is needed to create a single image. Most importantly, the rings used to create the diffractive optics come with a warning of post-operative glare or halos, which patients with severe glaucoma may be more prone to having.
Extended depth of focus IOLs (EDOF) also uses diffractive technology to elongate the primary focal point. This technology also comes with limitations: elongating the focal point also means less total light is dedicated to a single crisp image. EDOF lenses can carry warnings of a post-operative loss of contrast sensitivity. Still, it is often well tolerated by glaucoma patients without significant visual field defect or loss of foveal sensitivity.
How to match glaucoma patients to the right IOL
With increasingly earlier diagnoses at earlier ages, a number of minimally invasive options to keep IOP under control, and an increased number of patients who value the quality of life, glaucoma patients deserve to be informed of the advanced technology IOL options that are available to them – with careful consideration of the risks and benefits attached. In light of this, we present a list of considerations to help determine what IOL best suits a glaucoma patient’s specific needs.
Understanding patient goals
Every patient will have different priorities or goals: for some, complete freedom from glasses is their only priority; others may want to reduce their dependence on spectacles but wish to minimize the risk of glares, haloes, or loss of contrast sensitivity. These different requirements call for different treatment options. To achieve the former reliably and practically, the use of multifocal IOLs or a blended vision approach would be the best option. For the latter, the EDOF selection would provide a good balance between the range of vision and the reduced multifocal-related risks.
Additionally, it is important to ensure that patients understand the difference between “spectacle freedom” and “spectacle independence.” It might be beneficial to discuss that the “spectacle independence” of the EDOF IOLs should provide a better “range of vision” compared with monofocal or their current experience with presbyopia, typically achieving an uncorrected vision for computer and dashboard distance.
What is most bothersome to the patient?
Similar to goals, it is important to understand what symptoms of cataracts are bothering the patient the most. A cortical cataract patient experiencing significant glare and halos at night preoperatively would likely not be pleased should they experience postoperative glare and halos after a multifocal IOL. Similarly, those with color desaturation or contrast loss may be disappointed by the results, especially at night, of an EDOF IOL. Alternatively, any patient with mild to moderate myopia or early presbyopia with sufficient near vision may be disappointed when only distance vision is achieved, even when sufficiently consulted.
Glaucoma severity and progression
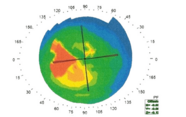
Those with mild or pre-perimetric glaucoma would benefit from multifocal or EDOF IOLs to a much greater degree than those with a small inferotemporal island that might not align with the refractive elements of the lens. Additionally, glaucoma that is so severe that vision now appears dim may not experience the same brightness or contrast sensitivity with an EDOF or multifocal compared with a monofocal. Similar to glaucoma severity, glaucoma progression must also be considered. A glaucoma progression analysis spanning 10 years with minimal change is much more reassuring for premium IOLs than a patient whose IOP is not well controlled on maximum medication with the risk of further surgery in the future.
Type of surgery
The type of surgery performed at the time of the cataract extraction may also factor into IOL choice. The majority of angle-based MIGS recovery and refractive outcomes are nearly identical to cataract surgery alone. Different types of glaucoma often inform the anatomy of the eye. For example, those with pseudoexfoliation or traumatic glaucoma may have areas of zonular weakness that could increase the risk of complications during the cataract extraction as well as postoperative decentration or postoperative tilt. To a greater degree than monofocals, premium IOLs are reliant on proper centration of the eye’s optical system for maximal effect of the diffractive elements. If this cannot be reasonably guaranteed due to underlying pathology, monofocal choices are likely safer – but this must be decided in conversation with the patients.
Retinal disease and IOLs
There is limited evidence that patients with retinal disease should be discouraged from multifocal IOLs. Although patients who have mild eye diseases, including age-related macular degeneration, would likely benefit from an EDOF IOL, the same cannot be said for any patients suffering from subfoveal or active macular pathology. Instead of benefiting their vision, the premium IOLs could hinder vision further by the parsing of available light. Patients with high axial myopia may have an increased risk of TORIC IOL rotation in the immediate postoperative period. Use of capsular tension ring, ensuring complete removal of viscoelastic from behind the IOL, avoidance of overinflation of the eye at the conclusion of the case, activity precaution on the day of surgery, as well as discussion of possibly needing an IOL rotation procedure would be prudent.
Lens exchanges
The final thing to consider is that surgeons offering multifocal, EDOF, or even toric IOLs should be comfortable with lens exchanges and have the ability to offer refractive laser enhancement at no additional cost.
On balance…
Although it may be safer to avoid implanting premium IOLs in all patients with glaucoma, this may significantly hinder the opportunity to gain spectacle freedom and increased quality of life gained by premium IOLs in stable, mild to moderate glaucoma patients. Some of the happiest and most grateful glaucoma patients are those who underwent a successful MIGS combined with premium IOL. As long as both the surgeon and the patient understand the risks, benefits, and alternatives to specific treatment options, it is important that glaucoma patients are offered the same opportunities for spectacle freedom and independence as any other cataract patients.
Matthew Hirabyashi, Resident at the University of Missouri, Columbia
Jella An, the Vice Chair for the Wilmer Eye Care Network at the Wilmer Eye Institute, Baltimore