Treating OSD with Amniotic Membranes
Why amniotic membrane therapy is an increasingly popular option for treating ocular surface disease
Zarmeena Vendal | | 5 min read | Discussion

Credit: Headshot supplied by Zarmeena Vendal
Because of its regenerative properties, ophthalmologists are increasingly using amniotic membrane therapy to treat ocular surface disease (OSD) (1-4). The most common forms of OSD are blepharitis and dry eye disease (DED), which may be related to meibomian gland dysfunction (MGD) and reduced tear production, among other factors (5). If left untreated, OSD may cause irreversible damage to the ocular surface, but early intervention can prevent progression to a severe and possibly difficult-to-manage disease state.
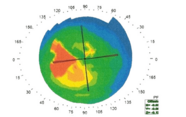
Over the last decade or so, we’ve seen substantial advances in diagnosing OSD. Beyond patient-reported symptoms and clinical observations at the slit-lamp, we have tools that can enable earlier detection and intervention, including infrared meibography and point-of-care tests to measure tear film osmolarity and matrix metalloproteinase-9. These tests can reveal signs of OSD even before patients notice symptoms, allowing for earlier diagnosis and improved outcomes (1,6,7). Even a small observable change on the ocular surface, such as punctate corneal staining, can be a critical sign of early-stage OSD and warrant treatment (1,8).
OSD treatment is based on severity and underlying etiologies and may include preservative-free eye drops, immunomodulators, topical antibiotics, warm compresses, lid scrubs, and intense pulsed light therapy. In instances of corneal epithelial damage, adjunctive amniotic membrane therapy may be necessary (1,5).
Amniotic membranes can be used as temporary grafts or substitutes for basement membrane to heal and restore damaged ocular tissue (3). Cryopreserved amniotic membrane (CAM; Prokera, BioTissue) offers more regenerative benefits over dehydrated tissues due to the healing benefits of the live protein matrix and structural integrity of the basement membrane. I regularly use CAM due to its ease of placement and reliable ocular surface recovery for patients. (2,9,10).
CAM treatment is beneficial for mild, moderate, and severe OSD, and early initiation often leads to favorable clinical responses. CAM also has utility in repairing the ocular surface prior to cataract surgery and resolving punctate keratitis associated with the use of topical glaucoma medications.
CAM for glaucoma medication relief
Studies show that more than half of patients who are prescribed glaucoma medications will develop some form of OSD (11), with nearly 90 percent showing evidence of abnormal tear quality (12,13). As a result, many patients with glaucoma also experience chronic, debilitating DED. Treating OSD in our glaucoma patients became a practice priority for us after one of our patients with significant corneal changes due to her glaucoma medications remarked that she would “prefer to go blind rather than continue with the side effects” induced by her eye drops. I realized at that moment, that as providers, it is equally our responsibility to treat our patients’ glaucoma and subsequent OSD.
As a result, I presented our practice data at ASCRS from a retrospective chart review of patients who were treated with CAM therapy for chronic DED induced by long-term use of glaucoma medication. For 100 percent of these patients, a single treatment with CAM – five days of corneal placement – resulted in improved signs and symptoms of DED for up to five months post-therapy (14). They all reported improvements in DED symptoms, pain, and quality of life after CAM treatment, and their corneal staining improved.
Applying CAM in clinical practice
The first step to incorporating regenerative therapy into practice is to identify signs of OSD in all patients, with knowledgeable staff and OSD questionnaires. Once OSD has been diagnosed, my staff advises patients that CAM therapy may improve their dry eye symptoms and is covered by most insurances (15).Typically, good candidates for CAM therapy are highly motivated to resolve their symptoms.
Prokera is a CAM product that is prepared as a disc and retained in a polycarbonate ring so that it can be applied much like a scleral contact lens. First, I instill a topical anesthetic; then, I open the package and rinse the membrane with sterile saline solution to remove extra preservation media. Inserting the membrane under the top and bottom eyelid, as with a contact lens, I use tape-tarsorrhaphy to keep the CAM centered and minimize discomfort. Five days later, the patient returns to the office for CAM removal.
My practice has a clinic dedicated to treating dry eye where seasoned technicians and staff optometrists are trained in placing, removing, and discussing CAM. We counsel patients that CAM therapy may cause some stinging, discomfort, or foreign body sensation during the five-day course of treatment. But we also explain the regenerative healing properties and improvement in symptoms following CAM therapy (16). Given our recent success in treating patients who have glaucoma medication induced OSD with CAM, we are now proactively educating our glaucoma patients about their OSD, and many of these patients are seeking CAM therapy to improve their symptoms and quality of life.
Takeaways
Intervening early with CAM can help restore ocular surface integrity in a variety of OSDs. Talking with patients about how CAM works and its potential to improve symptoms and reduce the risk of disease progression is helpful. Training clinical staff on CAM insertion, removal, and counseling can also help optimize integration of CAM into practice workflows. Ultimately, our patients’ quality of life can be truly improved with this therapy.
- CE Starr et al., “An algorithm for the preoperative diagnosis and treatment of ocular surface disorders,” J Cataract Refract Surg., 45, 669 (2019). PMID: 31030780.
- A Paolin et al., “Amniotic membranes in ophthalmology: long term data on transplantation outcomes,” Cell Tissue Bank, 17, 51 (2016). PMID: 26162811.
- A Gheorghe et al., “New clinical application of amniotic membrane transplant for ocular surface disease,” J Med Life, 9, 177 (2016). PMID: 27453750.
- P Gera et al., “Preparation and uses of amniotic membrane for ocular surface reconstruction,” Indian J Ophthalmol., 71, 3119 (2023). PMID: 12355703.
- L Jones, et al., “TFOS DEWS II management and therapy report,” Ocul Surf., 15, 575 (2017). PMID: 28736343.
- D Nicholas, W Gillian, “Meibomian gland imaging: a review,” African Vision and Eye Health, 74, 1 (2015). DOI: 10.4102/aveh.v74i1.12.
- WW Binotti, “A review of imaging biomarkers of the ocular surface,” Eye Contact Lens, 46 Suppl 2 (Suppl 2): S84(2020). PMID: 31833999.
- K Tsubota et al., “Defining dry eye from a clinical perspective,” Int J Mol Sci., 21, 9271 (2020). PMID: 33291796.
- M Cooke et al., “Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/chorion tissue,” J Wound Care, 23, 465 (2014). PMID: 25296347.
- MT Rodríguez-Ares et al., “Effects of lyophilization on human amniotic membrane,” Acta Ophthalmol., 87, 396 (2009). PMID: 18937812.
- X Zhang et al., “Ocular surface disease and glaucoma medications: a clinical approach,” Eye Contact Lens, 45, 11 (2019). PMID: 30199425.
- N Ruangvaravate et al., “High prevalence of ocular surface disease among glaucoma patients in Thailand,” J Ocul Pharmacol Ther., 34, 387 (2018). DOI: 10.1089/jop.2017.0104
- NR Betancourt et al., “Ocular surface disease prevalence in glaucoma patients in a high referral ophthalmology center in Mexico City,” Invest Ophthalmol Vis Sci., 54, 4342 (2013). PMID: 18703943.
- Z Vendal, “Management of glaucoma medication induced dry eye disease with self-retained cryopreserved amniotic membrane,” Journal of Dry Eye and Ocular Surface Disease, 5, E28 (2022). DOI: 10.22374/jded.v5i1.41.
- Corcoran Consulting Group, Reimbursement for Prokera. CorcorancCG.com. Published on August 8, 2022. https://www.corcoranccg.com/products/faqs/prokera/
- BioTissue, Prokera Insertion Guide. BioTissue.com. https://biotissue.com/support/product-inserts-guides/
Zarmeena Vendal, MD, founder of Westlake Eye Specialists, is a fellowship trained Glaucoma specialist, cataract, and refractive surgeon. She has practiced for over 15 years in Austin, TX. Financial disclosures: Alcon, Bausch & Lomb, J&J,Ocular Theraputix, RxSight, Sight Sciences.