Through the Lens
Sitting Down With… Ursula M. Schmidt-Erfurth, Professor and Chair of the Department of Ophthalmology at the Medical University of Vienna
Jamie Irvine | | 8 min read | Interview

Credit: Headshot supplied by Ursula M. Schmidt-Erfurth
How and why did you become an ophthalmologist?
The significance of visual perception cannot be overstated; it constitutes 90 percent of our sensory input. From the way we dream to understanding the emotions of others, our existence is innately tied to what we see. If you consider our perception of reality, for example, this is almost entirely driven by our personal, seen experiences. What someone sees as blue, another might perceive as green – and it is this convergence of objectivity and subjectivity that has held my attention across the years.
How did you shift gears from developing photodynamic therapy for AMD to the application of artificial intelligence?
Photodynamic therapy was a big step away from burning the retina at the affected area seen on angiography. The old rule was: if it shows up on angiography, burn it with a laser. But the bright spot becomes a dark spot, which is, of course, a scar and loss of retinal function. In my mind, there had to be alternative approaches.
After searching through the literature for other pathological vessels that can be closed, I came across photodynamic therapy. At the time, this method was used against tumors by occluding their vessels and injecting dye into the vasculature. It is activated by light, which causes the internal wall of the vessels to become damaged, meaning they don't leak any more or continue to grow. This was a huge step.
It was my first patent – acquired with my team at Harvard – and it shaped the treatment of age-related macular degeneration (AMD) for 10 years (from 1996 to 2006), resulting in millions of people treated.
Then, anti-VEGF therapy became available. The breakthrough was realizing that while medication could be effective, it necessitated regular invasive injections into the eye (given the chronic nature of the disease). Not long after this insight, I established a reading center dedicated to analyzing images from clinical trials, particularly those of the retina, to assess the efficacy of various substances. Over time, injections of these substances – now commonly used in intravitreal therapy – have become one of the most prevalent medical interventions, administered millions of times worldwide. With numerous substances and biosimilars now on the market, the reading center played (and still plays) a crucial role in evaluating their impact on macular disease through large-scale trials involving thousands of patients globally. This involves extensive image analysis, including three-dimensional volumes in randomized controlled trials.
We became a hub for image analysis crucial to the regulatory approval in a vast market. Operating from Vienna, Austria, we embraced digital medicine early on, delving into digital image analysis, and harnessing insights from extensive datasets. “Big data” led to the establishment of the Laboratory for Ophthalmic Image Analysis (OPTIMA, a) computer science group in 2013, spearheaded by true artificial intelligence (AI) experts, not just clinicians with a passing interest in IT. Our focus shifted towards developing algorithms capable of pinpointing disease biomarkers in the retina with unmatched precision, speed, and reproducibility. Currently, my primary focus lies in leveraging AI for the diagnosis and treatment of retinal diseases in the real-world clinical practice.
How might AI look a few years down the line?
When I first started my academic career, I thought AI would be the most intriguing area of research – and my experiences in the lack of diagnostic objectivity and reliability during medical school and residency only served to confirm this. Even now, my interest with the subject remains undiminished. Waiting for something “down the line” isn’t necessary; it is already here.
It may surprise you to learn that blindness is still a major challenge in modern societies – the rates for irreversible visual loss have substantially increased over the last 20 years. In fact, we know that the loss of visual acuity impacts a person’s life more than having cancer. It changes every aspect of your existence immediately and irreversibly; it makes individuals totally dependent on others, starving any level of autonomy you may have had previously. I can’t stress the extent of this issue – and I believe that AI is integral to efficiently addressing this enormous challenge.
AI is inherently reproducible and, therefore, it allows for a shared care model where community-based optometrists, opticians, who frequently encounter individuals requiring reading glasses, and even pharmacists, who cater to elderly patients in need of various medications, can all participate in disease screening efforts.
Over the next one to three years, we anticipate a scenario where every eye doctor can readily use a validated algorithm to accurately measure fluid levels in exudative macular disease and assess photoreceptor loss in geographic atrophy; this standardized approach will generate insights that can act as a therapeutic guideline for the identification of optimal drugs.
How might AI impact teaching and learning in the future?
AI has the capacity to bring healthcare professionals together; it is not something we should fear. It sets the stage for improved communication and insights that will more and more change our understanding of ophthalmic treatment. But it needs big data. In medicine, we need to pool together our images and learn from the experiences of countless patients, moving beyond anecdotal evidence to evidence-based practices backed by the data of millions. Shared care is bringing early diagnoses to everyone – even the people that wouldn’t have time or means to see an eye doctor. And because AI is not as expensive as a human expert, it is also not as limited.
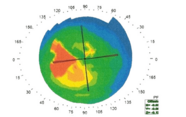
AI significantly improves our understanding of disease mechanisms. Take geographic atrophy, for example. An AI-based analysis of trials for this disease showed that the retina progressively thins, leading to the dropout of photoreceptors before pigment loss becomes clinically apparent. This discovery fundamentally changed our understanding and educational approach to AMD. Moreover, the digital era facilitates instantaneous sharing of insights and knowledge through platforms like virtual conferences. The exchange of insights owes much to AI’s ability to vividly illustrate complex features and phenomena and detect associations.
Can you tell us about your current role and responsibilities?
My role encompasses a broad spectrum of responsibilities spanning clinical care and department functionality – but each day is different. On some days, I may oversee the operational aspects of the department, ensuring that the highest standards are maintained in patient diagnosis and treatment. Then I am performing surgical interventions. On others, my focus will lie on medical cases referred to me for specialized attention. It’s very rarely repetitive – and there is always something new to learn.
I also have the chance to shape the scientific progress of our department. This includes assembling and nurturing teams of individuals, who each contribute their skills and perspectives to yield the highest standard research. Today, I am proud to say that we have a high diversity index, covering 22 nations while maintaining a positive gender balance. It goes without saying that sustaining a high level of scientific rigor beyond all borders is paramount.
Securing funding through grant writing is another facet of my position – and it is one of the most time-consuming tasks on my to-do list. At the University in Vienna we receive no financial support for research in terms of manpower or budget, so, if you want to provide an efficient scientific output, a do-it-yourself mentality is necessary.
What challenges do we continue to face in ophthalmology?
There are multiple diseases we cannot manage sufficiently at the moment, but the big elephant in the room is geographic atrophy or dry AMD. Managing dry AMD is akin to addressing Alzheimer’s disease, yet we’ve seen notable progress in this area recently – just a few months ago, the FDA approved the first two substances capable of treating geographic atrophy. These treatments are now available in the US, with regulatory approval submissions ongoing in Europe through the EMA after demonstrating relevant therapeutic effect.
Moving forward, our focus will shift towards employing effective diagnostic modalities to identify patients who benefit most from these treatments. It is important to recognize that this treatment may not be universally effective, as disease activity is the base for therapeutic benefit.
However, through post hoc analysis, specific markers indicating disease activity and treatment responsiveness have been identified. This analysis is heavily reliant on AI-based image analysis of OCT images – an area in which we specialize. As a result, my team and I have spent a long time making our algorithms readily available for use by healthcare providers in the clinic as well as the community.
In fact, the team that branched off from the university has made notable progress within the last two years. For example, they successfully delivered algorithms for fluid and geographic atrophy detection into the hands of eye doctors in Europe, securing MDR approval. These achievements are now in submission to the FDA.
Could you tell us about your proudest achievements?
Generally, the past is encouraging – because it serves as a foundation for future growth. With each insight comes a question, which leads to another answer. Rather than pinpointing a singular highlight, I embrace the ongoing evolution of ideas. It is a continuous, dynamic process – or a collaborative effort where minds engage in dialogue, exchanging expertise and inspiration. This interconnectedness and exchange of knowledge have always fuelled my passion and continue to do so today.
What career advice do you have for the rising stars of ophthalmology?
I would refrain from advising someone to build – or care – about their “career.” Follow your passion and find growth in the things that matter to you. Don’t fixate on side-effects like awards to define your professional life either. Instead, pursue what genuinely interests you, even if it is challenging. Seek advice, gather ideas, and collaborate with others who share the same spirit and can offer valuable insights. Progress may be gradual, and there will be times when things move slowly, but don’t let that deter you. Ultimately, find fulfilment in what you do and surround yourself with a supportive community that you enjoy being a part of.
Associate Editor | The Ophthalmologist and The New Optometrist.