A common sleeping habit may be inadvertently worsening intraocular pressure (IOP) control in patients with glaucoma, according to a new study published in the British Journal of Ophthalmology. The researchers – based at Zhejiang University, China – reported that sleeping with the head elevated on multiple pillows – a posture many patients adopt for comfort or reflux – is associated with higher nocturnal IOP, greater 24-hour IOP fluctuation, and significantly reduced ocular perfusion pressure (OPP).
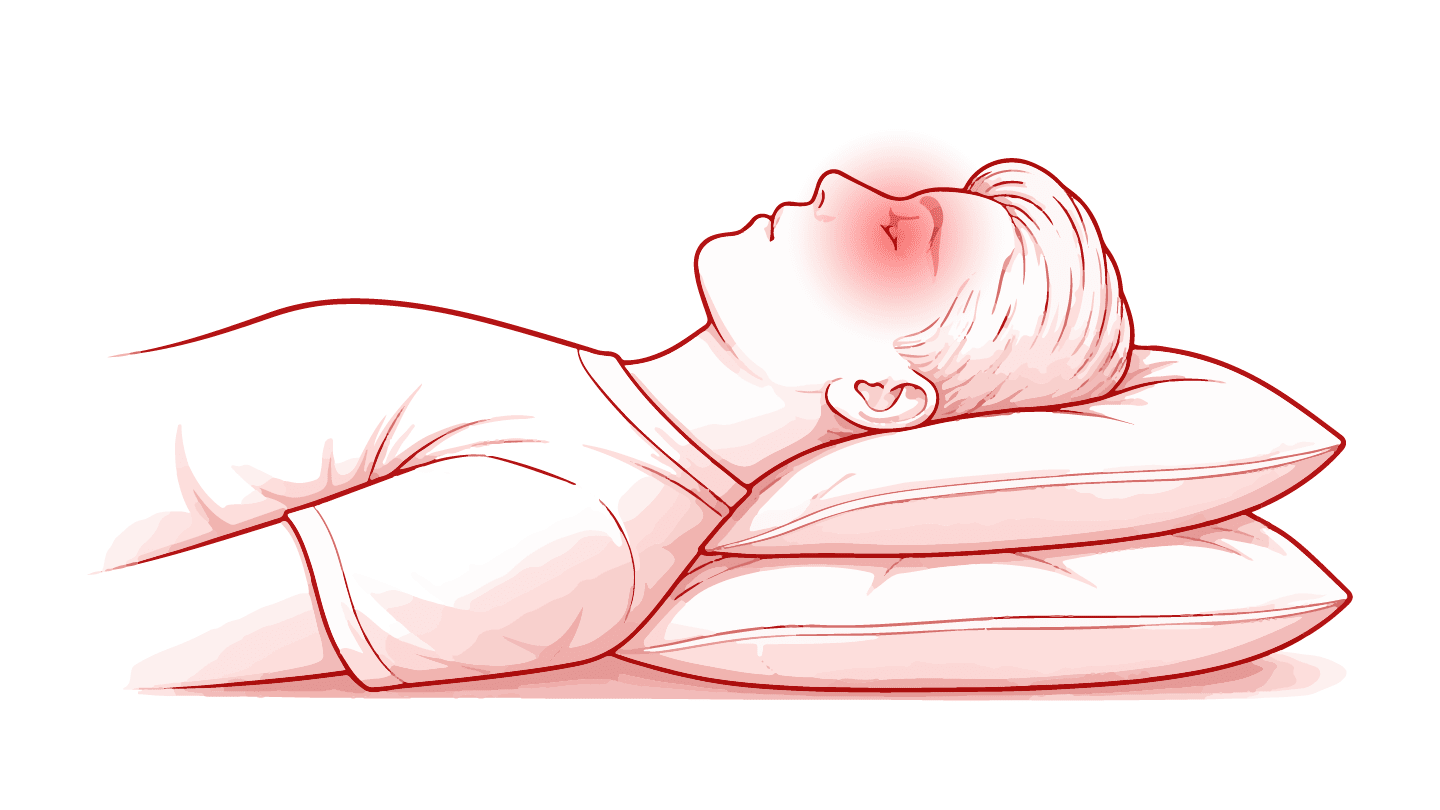
The study enrolled 144 glaucoma patients who underwent standardized 24-hour IOP monitoring. Nocturnal measurements were taken first in a supine position and then after head elevation of approximately 20–35 degrees using two standard pillows, reflecting a realistic “high-pillow” sleeping posture. The investigators found that IOP was significantly higher in this high-pillow position than when patients lay supine.
On average, IOP increased by 1.6 mm Hg with head elevation, and nearly two-thirds of patients experienced a measurable rise. This posture was also associated with larger overall diurnal IOP fluctuations, and a significant reduction in OPP – an important surrogate marker for ocular blood flow. Reduced OPP has been implicated in glaucoma progression, raising concerns about the long-term impact of this sleeping position.
To explore a possible mechanism, the researchers conducted jugular vein ultrasonography in healthy volunteers. Imaging showed significant narrowing of both the internal and external jugular veins in the high-pillow position, accompanied by increased blood flow velocity – findings consistent with mechanical venous compression. The authors suggest that neck flexion caused by pillow elevation may impair venous drainage, increasing episcleral venous pressure and limiting aqueous humor outflow.
While the researchers stress that further longitudinal studies are needed to develop a more comprehensive understanding of the dynamics involved in postural IOP changes across glaucoma subtypes, their findings highlight a simple, modifiable behavior that may influence IOP control for patients with glaucoma.
The study enrolled 144 glaucoma patients who underwent standardized 24-hour IOP monitoring. Nocturnal measurements were taken first in a supine position and then after head elevation of approximately 20–35 degrees using two standard pillows, reflecting a realistic “high-pillow” sleeping posture. The investigators found that IOP was significantly higher in this high-pillow position than when patients lay supine.
On average, IOP increased by 1.6 mm Hg with head elevation, and nearly two-thirds of patients experienced a measurable rise. This posture was also associated with larger overall diurnal IOP fluctuations, and a significant reduction in OPP – an important surrogate marker for ocular blood flow. Reduced OPP has been implicated in glaucoma progression, raising concerns about the long-term impact of this sleeping position.
To explore a possible mechanism, the researchers conducted jugular vein ultrasonography in healthy volunteers. Imaging showed significant narrowing of both the internal and external jugular veins in the high-pillow position, accompanied by increased blood flow velocity – findings consistent with mechanical venous compression. The authors suggest that neck flexion caused by pillow elevation may impair venous drainage, increasing episcleral venous pressure and limiting aqueous humor outflow.
While the researchers stress that further longitudinal studies are needed to develop a more comprehensive understanding of the dynamics involved in postural IOP changes across glaucoma subtypes, their findings highlight a simple, modifiable behavior that may influence IOP control for patients with glaucoma.
